Dresden, 01.12.2017
Novel transcriptomic signature of type 2 diabetic islets identified
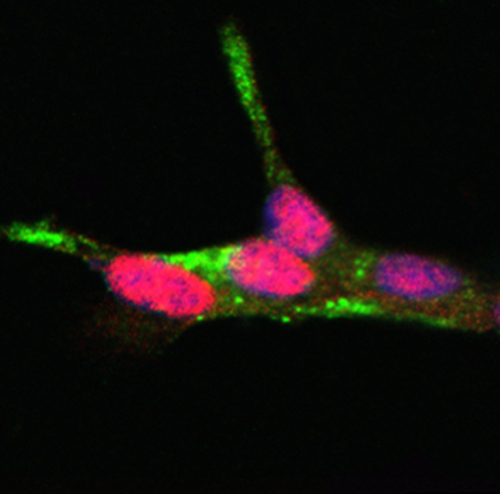
Type 2 diabetes, which affects >0.5 billion people worldwide, results from the inability of beta cells in the pancreatic islets to provide the body with enough insulin to maintain blood glucose levels within the range for a healthy life.
A collaborative study led by Prof. Michele Solimena at the Technische Universität in Dresden, Dr. Anke M Schulte at Sanofi in Frankfurt, Dr. Mark Ibberson at the Swiss Institute of Bioinformatics (Lausanne) and Prof. Piero Marchetti at University of Pisa as part of the EU-Innovative Medicine Initiative (IMI) research consortium IMIDIA has identified a novel cluster of dysregulated genes in the pancreatic islets of patients with type 2 diabetes. These findings are now published in the scientific journal Diabetologia.
The goal of the IMIDIA consortium, which involved 14 European academic institutions, large pharma companies and biotech firms from 02.2010 until 09.2016, was to identify novel paths for the regeneration, maintenance and protection of insulin-producing pancreatic beta cells as a mean to expedite the discovery of more effective strategies to prevent and treat diabetes. A main task of the IMIDIA consortium was to define which genes are abnormally expressed in islet beta cells of diabetic subjects compared to islet beta cells of non-diabetic subjects. The altered expression of these genes could account for beta cell failure in diabetes. For the first time, the investigators based their comparative gene expression analysis not only on islets collected from non-diabetic and diabetic organ donors, for which the availability of clinical information is limited, but also on islets from patients undergoing pancreatic surgery. For the latter subjects in depth medical information was available and the diabetic status could be accurately assessed immediately prior to surgery. This approach enabled therefore the assembly of the largest collection of islets from non-diabetic and diabetic subjects, but also access to islets from prediabetic individuals. The investigators identified in this way nineteen genes the expression of which was altered in islets of both diabetic organ donors as well as diabetic surgical patients. Notably, nine of these nineteen genes had never been shown previously to be dysregulated in diabetic islets. On the other hand, the study could not find evidence for any of these genes to be dysregulated in islets of prediabetic subjects, hence suggesting that their altered expression is a consequence rather than the cause of beta cell failure in diabetes. Hence, future studies shall be devoted to discover which genes are dysregulated prior to the demise of the beta cells. For this purpose, more islets must be collected from prediabetic subjects and this is precisely one of the main tasks pursued by the recently launched EU-IMI consortium RHAPSODY, which includes all four teams leading the present IMIDIA study as partners.
“We believe that our data provides novel molecular insights into what is going wrong in diabetic beta cells and sets new standards for how studies in this field shall be carried out in the future. Ultimately, we are confident that our approach will provide a new view for how exposure of beta cells to nutrient overload wears their function overtime, hence impairing their ability to satisfy the excessive demand of insulin to maintain metabolic homeostasis” says Prof. Michele Solimena, one of the four leading investigators of this study
About IMIDIA:
IMIDIA (“Innovative Medicines Initiative for Diabetes”, www.imidia.org) is a public private consortium funded by the Innovative Medicines Initiative (IMI) and is led by Sanofi-Aventis, Servier and the University of Lausanne. Leading European experts from 14 academic institutions, eight pharmaceutical research organizations and one biotech company in the area of pancreatic beta cells officially joined their forces within the IMIDIA project to fight diabetes. IMIDIA is working on the generation of novel, patient centric tools, biomarkers, and fundamental knowledge on beta cell organization to accelerate the path to improved diabetes management. It is a unique collaboration of leading research groups in Europe focusing on the necessary innovation tightly coupled with the applications and evaluation of these results to develop new diagnostics, prognostics and therapeutics. Approximately 100 researchers operating in six different scientific work packages focus on novel approaches e.g. imaging biomarkers, systems biology and pathway analysis with the goal of developing patient relevant disease models in vitro and in vivo as well as biomarkers to monitor disease progression and treatment.
IMIDIA participants were AstraZeneca, Boehringer Ingelheim, the French Atomic Energy Commission (CEA), Hannover Medical School (MHH), Imperial College London, Lilly, the National Centre for Scientific Research (CNRS), the National Institute of Health and Medical Research (INSERM), Novartis, Novo Nordisk, Roche, Sanofi-Aventis, Sarl Endocells, Servier, SIB Swiss Institute of Bioinformatics, Vrije University of Brussels, Technische Universität Dresden, University of Geneva, University of Lausanne, University Paris Diderot and University of Pisa. Additional financial support for this study was provided by the German Center for Diabetes Research (DZD e.V.), which is supported by the German Ministry for Education and Research; the Italian Ministry of Education and Research, and by the Wellcome Trust, the Medical Research Council and the Royal Society in the UK.
Original Publication:
Solimena et al. Systems biology of the IMIDIA biobank from organ donors and pancreatectomised patients defines a novel transcriptomic signature of islets from subjects with type 2 diabetes. Diabetologia, 2017. DOI: https://doi.org/10.1007/s00125-017-4500-3.
Press contact

Birgit Niesing
niesing(at)dzd-ev.de
+49 (0)89 3187-3971
 |
