Research
A future without diabetes – that is the ambitious goal of the DZD. To realize this vision, the DZD combines the expertise of leading German research institutions and universities in the field of metabolic and diabetes research.
Main research topics – DZD Academies
The DZD is working on the most pressing issues in diabetes research. # What influence do liver or brain have on diabetes? # How do environmental factors such as diet affect the activity level of genes? # How can beta cells be protected? # What other diseases are associated with diabetes? # How can metabolic disease be prevented? # How does the autoimmune disease type 1 diabetes develop?
In order to be able to investigate these questions, the DZD is focusing on the following research topics (DZD Academies):
![]() Type 1 diabetes – prevention of the autoimmune disease
Type 1 diabetes – prevention of the autoimmune disease
Development of a therapy that regulates the immune system in a way that prevents the destruction of beta cells.
![]() Prevention of type 2 diabetes
Prevention of type 2 diabetes
The aim is successful personalized diabetes prevention.
![]() Complications of diabetes
Complications of diabetes
Diabetes can lead to various serious complications. To avoid or delay such consequences in the future, it is important to identify which patients have a high risk of complications.
![]() The influence of genetics and epigenetics on the development of diabetes
The influence of genetics and epigenetics on the development of diabetes
Research into the genetic and epigenetic mechanisms in metabolism in animal models and in human samples.
![]() Causes and treatment of non-alcoholic fatty liver disease
Causes and treatment of non-alcoholic fatty liver disease
Obesity and type 2 diabetes are closely related to non-alcoholic fatty liver disease (NAFLD) and steatohepatitis (NASH).
![]() Insulin action and resistance in the brain
Insulin action and resistance in the brain
Studies have shown that insulin resistance of certain brain areas has a negative effect on metabolism.
![]() Protection and regeneration of beta cells
Protection and regeneration of beta cells
The elucidation of the mechanisms of destruction and/or functional impairment of beta cells as a prerequisite for new therapeutic approaches.
Interdisciplinary collaboration – conducting research together
How does diabetes mellitus develop? What factors contribute to this? How can the disease be prevented, treated or even cured? No research group or institution alone can find the answers to these questions. Only an integrative research approach that unites different disciplines can decipher the complex processes involved in the development of diabetes mellitus. The special added value of the DZD is based on its broad professional expertise, the cross-departmental and cross-institutional collaboration of basic researchers, clinicians, epidemiologists and health care researchers, as well as state-of-the-art research infrastructures.
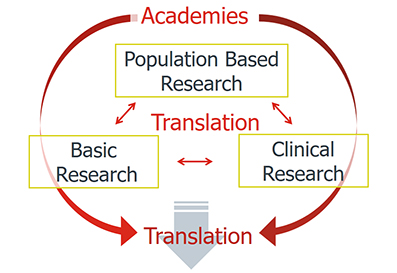
From the lab to the patient – translational research
The aim of this close collaboration is to transfer the findings and results of diabetes research as quickly as possible from the laboratory to clinical studies and then to the patient (from bench to bedside). In translational research, the findings are not only transferred in one direction – observations from the clinic are also incorporated into basic research.
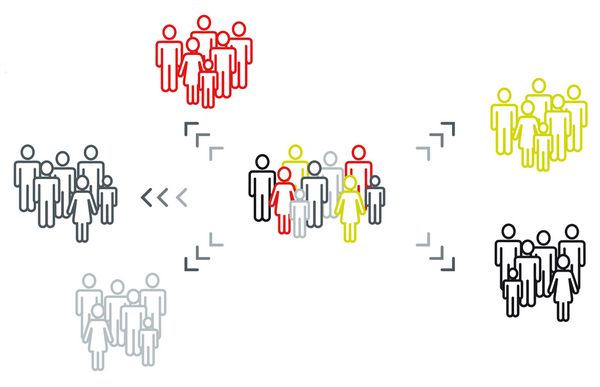
Multicenter studies
In order to be able to develop precision prevention and therapy measures, i.e. the right treatment for the right patient group at the right time (Precision Medicine), the DZD has set up large-scale multicenter studies. The Germany-wide cooperation in the research network makes it possible to initiate such large studies and to recruit the necessary participants. Currently over 5,000 people are participating in the studies.
Innovative infrastructures
For successful translational biomedical research, state-of-the-art technological platforms are a basic prerequisite. Therefore, the DZD specifically strengthens the development of research infrastructures for key technologies at the DZD locations and establishes central service facilities.
Prof. Dr. Martin Hrabé de Angelis, DZD Board of Directors: DZD Research Program
Here is a video deposited in Vimeo. With your consent, a connection to Vimeo is established. Vimeo may also use cookies. For more information, click here: Vimeo Privacy Policy.
Talk at the 10th anniversary celebration of the DZD on June 24, 2019 in Berlin (in English).
Overview

10 years of translational diabetes research at the DZD
Donations
If you would like to support our research work, we would be pleased to receive your donation.
Thank you for your support!
Locations of the DZD Partners
German Diabetes Center in Düsseldorf
German Institute of Human Nutrition in Potsdam-Rehbrücke
Helmholtz Zentrum München – German Research Center for Environmental Health
Institute for Diabetes Research and Metabolic Diseases of the Helmholtz Zentrum München at the Eberhard-Karls-University of Tuebingen
Paul Langerhans Institute Dresden of the Helmholtz Zentrum München at the University Hospital and Faculty of Medicine Carl Gustav Carus of TU Dresden
In order to complete and strengthen the scientific competence the DZD integrates single diabetes research scientists and groups at the Universities in Heidelberg, Cologne, Leipzig, Lübeck and Munich as associated partners.
DZD scientists use the following affiliation in scientific publications
Deutsches Zentrum für Diabetesforschung (DZD), Ort* bzw.
German Center for Diabetes Research (DZD), Site*
* if required by the journal

